Will that CT scan be the death of you?
A new study suggests that CT scans could account for 5% of all cancer diagnoses annually.
A CT scan expose you to radiation - equivalent to being a few miles from the epicentre of an atomic bomb going off - you knew that right? Well, you probably knew it involved some radiation, and that radiation is carcinogenic, but I doubt you knew how carcinogenic? A CT scan does involve a lot of ionizing radiation - equivalent to about 1000 dental x-rays or eating 50,000 bananas - ok, that last comparison is not particularly helpful, but it does serve to remind us that we are all exposed to some radiation every day, and often unlikely places, such as bananas, albeit in much, much, smaller doses. I’m getting these figures from Munroe’s excellent infographic (below). The infographic also tells us that the dose of radiation you receive during a chest CT is about equivalent to whiling an hour at away in downtown Chernobyl.
(Part of) Radiation dose chart figure by Randall Munroe - link here.
That’s interesting but what does it mean in terms of cancer risk. Enter a new study on CT scans and cancer risk - “Projected Lifetime Cancer Risks From Current Computed Tomography Imaging” by Smith-Bindman et al published in JAMA Internal Medicine. This kind of study has been done before, but this one is the most up to date and has very good data on the utilisation of CT scanning across different age groups, sex and the exposure of different organs that differ in their sensitivity to radiation induced damage. The projected cancer risks were derived by taking data on a lot of CT’s and running it through a risk calculator. The authors found that current (2023) CT use in the US could result in 100,000 cancers (about 5% of all cancer) annually. That is some claim. To put that into context, that would put it in the top three known causes of cancer, in amongst alcohol and excess body weight (see figure 2).
Figure 2: Estimated proportion and number of incident cancer cases attributable to evaluated risk factors in adults 30 years and older by sex, United States, 2019 (Islami et al, 2019).
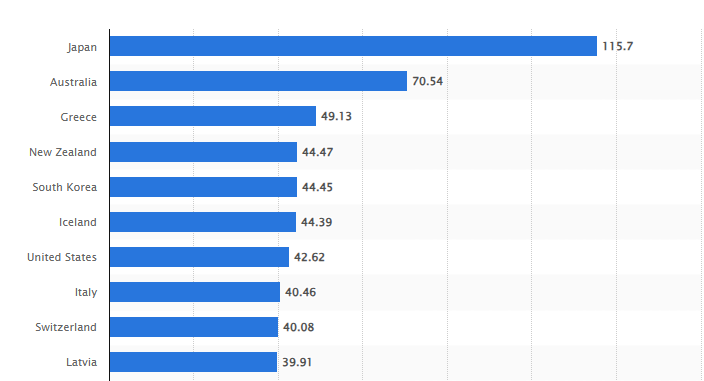
Part of the problem is of course that the US does a lot of CT examinations - 93 million were performed in 61 million patients in the US in 2023 according to the authors. To do a lot of scanning, you need a lot of scanners, and the US have a lot, but nowhere near as many as Japan, per head of population (see figure 3). The number of scans in in the US in 2023 is 30% higher than it was in 2007. Some of this shift is due to demographic shifts (that’s science speak for more old people around) but some of it is due to unnecessary scans. In the UK, we lag behind the US (and most of the developed world) in the number of CT scanners per head (The UK has 10 per million, the US has 43). I am pretty sure we lag behind the US in both the number of scanners, and the amount of necessary and unnecessary CT scans, something the current administration is keen to address. The NHS needs to modernise or die says the now Health Secretary. Modernisation here means doubling the number of CT and MRI scanners in hospital. Doubling the number of CT scanners well might save the NHS, but if this paper has it right, it could kill you in the process.
Figure 3. Number of computer tomography (CT) scanners in selected countries as of 2023 (per million population). From Computer tomography scanners density by country 2023| Statista.
Is the science settled?
Let’s be clear, this study does projections based on population-level data and assumptions about radiation risk - it does not show a direct causal link between specific CT scans and individual cancer cases. It doesn’t attempt to apportion which cancers could have been caused by CT retrospectively – this is much harder to do. It’s not that this is not a good study, it looks to be very well done, it’s just that modelling studies often hinge on assumptions that if wrong, have devasting consequences for the results and seriously damage your chances of publishing your work in the most important journals.
The big assumption here is the risk from low-dose radiation (<100-200 mSv), which is extrapolated from the effects at higher doses. The conclusions of the paper hinge on the linear no threshold (LNT) model of carcinogenicity. The LNT model says there is no safe dose of radiation - the line of dose against risk is a straight line back to the origin (figure 4). Not everyone agrees with this, and there is an argument for a threshold which needs to be exceeded for radiation to cause cancer (linear threshold model). There is even an argument that low-dose radiation exposure is beneficial, not harmful - this is the hormesis model. I have no idea if anyone takes the supra-linear model seriously. If that model were true for radiation and cancer, then we would be in trouble!
Figure 4. Different dose-response models in risk assessments. Radiation exposure (x-axis) and overall risk (y-axis) (from Seong et al).
Although I haven’t done the calculations, anything other than the linear or supra-linear model would result in far fewer cancers than projected by Smith-Bindman. The hormetic model would even suggest that more CT’s equal fewer cancers. Siegel and Welsh argue that the LNT model is not biologically plausible and that a healthy normal body can deal with low-dose radiation induced mutations through a set of mechanisms called the adaptive response. This idea leads to the threshold model. There appears to be a consensus forming towards the linear no-threshold model, but not necessarily for the implications of such a model. For example, the International Commission on Radiological Protection (ICRP) thinks that the risk probably is proportional to dose and that there is no lower level at which the risk is zero, but at the same time cautions against risk projections based on large numbers of people receiving low doses due to uncertainties.
Benefit/Harm.
In the end, it all boils down to the risk/benefit trade off - like so much of medicine. I recall discussing the radiation risk from CTs with a Professor of Radiology at Oxford some years ago. We were working together on a research project where people with non-specific symptoms of cancer got rapid access to a low-dose whole-body CT scan (which is not standard in the UK) as well as other investigations. Some people questioned this approach and the risk from the CT, but he asserted, and I didn’t argue with him at the time, that there was no direct evidence of harm from diagnostic radiation, and anyway the benefits would outweigh any risk. As the number of people in our study turned out to have late-stage cancer and other serious illnesses, the radiation risk from CT was arguably balanced by expediting a diagnosis, which up to that point had not been made. However, when fewer people stand to benefit, as is often the case with population wide screening, the risk outweigh the benefit. I wonder if they need to revisit the benefit/harm balance for the national screening programme for lung cancer using CT as a result of this paper?
References.
Islami F, Marlow EC, Thomson B, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States, 2019. CA Cancer J Clin. 2024; 74(5): 405-432. doi:10.3322/caac.21858.
Smith-Bindman, R., Chu, P. W., Firdaus, H. A., Stewart, C., Malekhedayat, M., Alber, S., ... & Miglioretti, D. L. (2025). Projected lifetime cancer risks from current computed tomography imaging. JAMA Internal Medicine.
Seong KM, Seo S, Lee D, Kim MJ, Lee SS, Park S, Jin YW. Is the Linear No-Threshold Dose-Response Paradigm Still Necessary for the Assessment of Health Effects of Low Dose Radiation? J Korean Med Sci. 2016 Feb;31 Suppl 1(Suppl 1):S10-23. doi: 10.3346/jkms.2016.31.S1.S10. Epub 2016 Jan 28. PMID: 26908982; PMCID: PMC4756336.
Siegel JA, Welsh JS. Does Imaging Technology Cause Cancer? Debunking the Linear No-Threshold Model of Radiation Carcinogenesis. Technol Cancer Res Treat. 2016 Apr;15(2):249-56. doi: 10.1177/1533034615578011. Epub 2015 Mar 30. PMID: 25824269.